Could a seemingly simple medication hold the keys to understanding complex medical scenarios, and even, in some cases, the very end of life? The answer, as we delve into the world of barbiturates, particularly phenobarbital and pentobarbital, reveals a story of both therapeutic promise and potential controversy.
The journey of a drug through the human body is a fascinating interplay of absorption, distribution, metabolism, and excretion. Phenobarbital, a barbiturate with a history spanning decades, offers a clear illustration of these processes. Administered orally, it boasts an impressive bioavailability of approximately 90%. This means that a significant portion of the drug enters the bloodstream and becomes available to exert its effects. The peak plasma concentrations, often denoted as cmax, are typically achieved within eight to twelve hours after ingestion. But what truly defines a drug's presence in the body, and its duration of action, is its half-life.
Understanding the concept of half-life is crucial. It is the estimated time it takes for the amount of drug in the body to reduce by half. For phenobarbital, this time is approximately four days. This relatively long half-life contributes to its sustained effects and the need for careful consideration in dosage and potential withdrawal symptoms. Imagine taking 200mg of phenobarbital; four days later, 100mg would remain within the body. This extended presence in the system necessitates caution, especially concerning potential side effects and interactions with other substances.
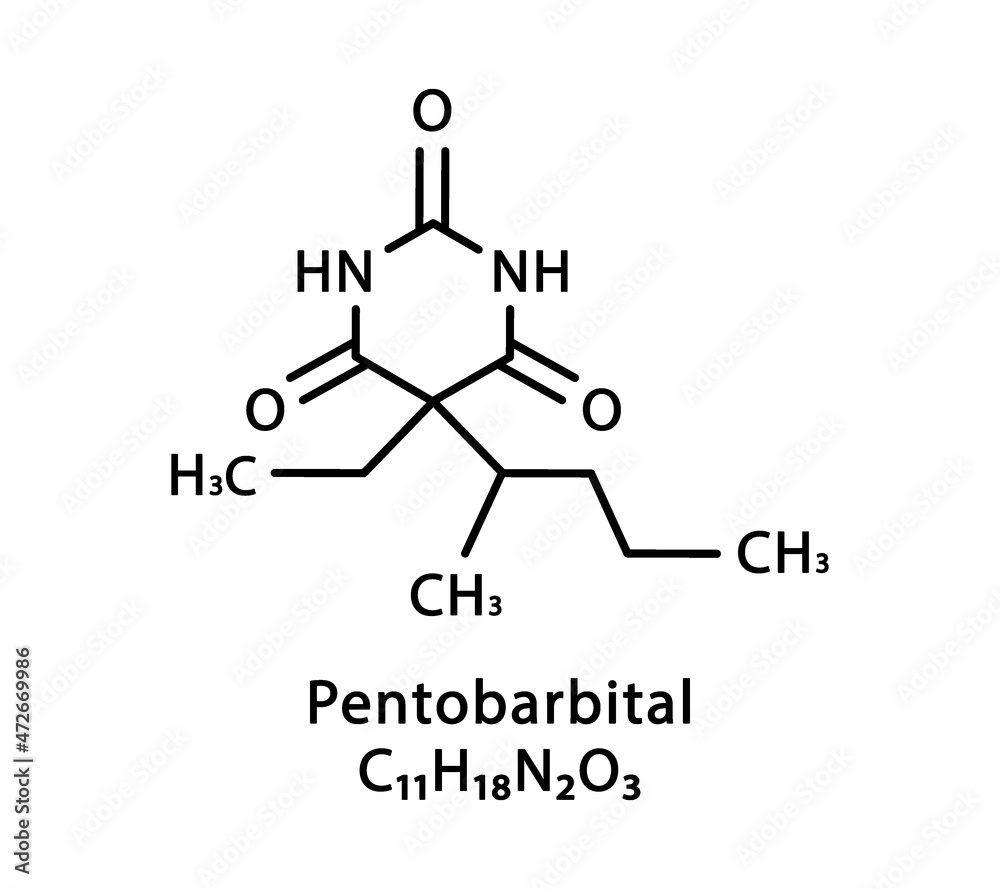
Pentobarbital, another barbiturate, shares some similarities with phenobarbital but often plays a distinct role. It is a fast-acting barbiturate that acts as a central nervous system depressant, which makes it useful as an anesthetic, a treatment for seizures, and in the medical field for euthanasia purposes. However, its use is far from uniform across the globe. In Germany, for example, pentobarbital is primarily reserved for veterinary medicine. Its use in humans raises ethical and legal questions, particularly in the context of assisted suicide and the death penalty. The sleepiness can be more intense if you receive pentobarbital (nembutal) after you've recently drank alcohol or taken other medications that can slow your body down, such as sedatives and opioids. The potential for serious side effects, including slow heart rate (bradycardia), low blood pressure (hypotension), and respiratory depression, underscores the importance of professional medical supervision.
The potential for dependence and withdrawal is a critical consideration with barbiturates, particularly pentobarbital. Abrupt cessation of the drug after prolonged use can trigger withdrawal symptoms, necessitating a cautious approach to discontinuation. The guidance of a medical professional is essential to manage withdrawal symptoms and avoid adverse effects. Common side effects of pentobarbital, such as nausea, vomiting, and constipation, can significantly impact a patient's well-being. Moreover, the risk of respiratory complications, including apnea and hypoventilation, highlights the need for careful monitoring, especially in vulnerable individuals.
Barbiturates, in general, are metabolized primarily by the hepatic microsomal enzyme system within the liver. The resulting metabolic products are then excreted from the body, predominantly through the urine and, to a lesser extent, through the feces. This metabolic pathway can be affected by other drugs or underlying medical conditions, potentially altering the duration and intensity of the barbiturate's effects. Dosage adjustments may be required for certain patients, particularly those receiving corticosteroids, which can affect the metabolism of barbiturates. Close monitoring of patients, especially those with asthma or other respiratory conditions, is crucial when initiating or adjusting barbiturate therapy. Furthermore, the effects of barbiturates may persist for up to two weeks after discontinuation, emphasizing the need for ongoing medical observation. The use of alcohol while taking barbiturates is strongly discouraged because it can exacerbate the central nervous system depressant effects and increase the risk of adverse events.
The use of pentobarbital is a subject of significant ethical and legal debate. It is a fast-acting barbiturate that acts as a central nervous system depressant. It is sometimes used as an anesthetic, to treat seizures, and in certain medical contexts, like euthanasia. However, its applications vary across different jurisdictions, and its use in assisted suicide and the death penalty raise significant ethical and legal concerns. In countries like Switzerland, it is a medication used in assisted suicide, while in the United States, it may be used in the execution of the death penalty. In Germany, pentobarbital is restricted to veterinary medicine.
The profound impact of barbiturates on the central nervous system underscores the importance of careful monitoring and informed medical decisions. The long half-life of phenobarbital, the potential for withdrawal with pentobarbital, and the metabolic pathways of these drugs are all vital considerations for both patients and healthcare providers. Understanding the intricate pharmacology of these medications allows for responsible and informed use, ensuring patient safety and well-being.
For more detailed information on the usage, side effects, and legal aspects of barbiturates, it is always recommended to consult a medical professional or refer to reputable sources.
| Drug Information: Phenobarbital and Pentobarbital | |
|---|---|
| Drug Name | Phenobarbital, Pentobarbital (Nembutal) |
| Drug Class | Barbiturates |
| Oral Bioavailability (Phenobarbital) | Approximately 90% |
| Peak Plasma Concentration (cmax) - Phenobarbital | 8 to 12 hours after oral administration |
| Half-Life (Phenobarbital) | Approximately 4 days |
| Metabolism | Hepatic microsomal enzyme system |
| Excretion | Urine (primarily), feces (less commonly) |
| Uses (Phenobarbital) | Anticonvulsant (seizure control), sedative |
| Uses (Pentobarbital) | Anesthetic, treatment of seizures, euthanasia (depending on region) |
| Potential Side Effects (Pentobarbital) | Slow heart rate (bradycardia), low blood pressure (hypotension), fainting (syncope), nausea, vomiting, constipation, apnea, hypoventilation. |
| Withdrawal Symptoms (Pentobarbital) | Possible if stopped abruptly after regular use; requires medical supervision. |
| Legal Status/Usage Variations |
|
| Cautions/Interactions |
|
| Reference Website | Drugs.com |