Could a seemingly innocuous infection in your mouth or throat potentially lead to a serious and often misdiagnosed illness? Actinomycosis, a rare bacterial disease, often presents with symptoms that mimic other conditions, making early detection a significant challenge.
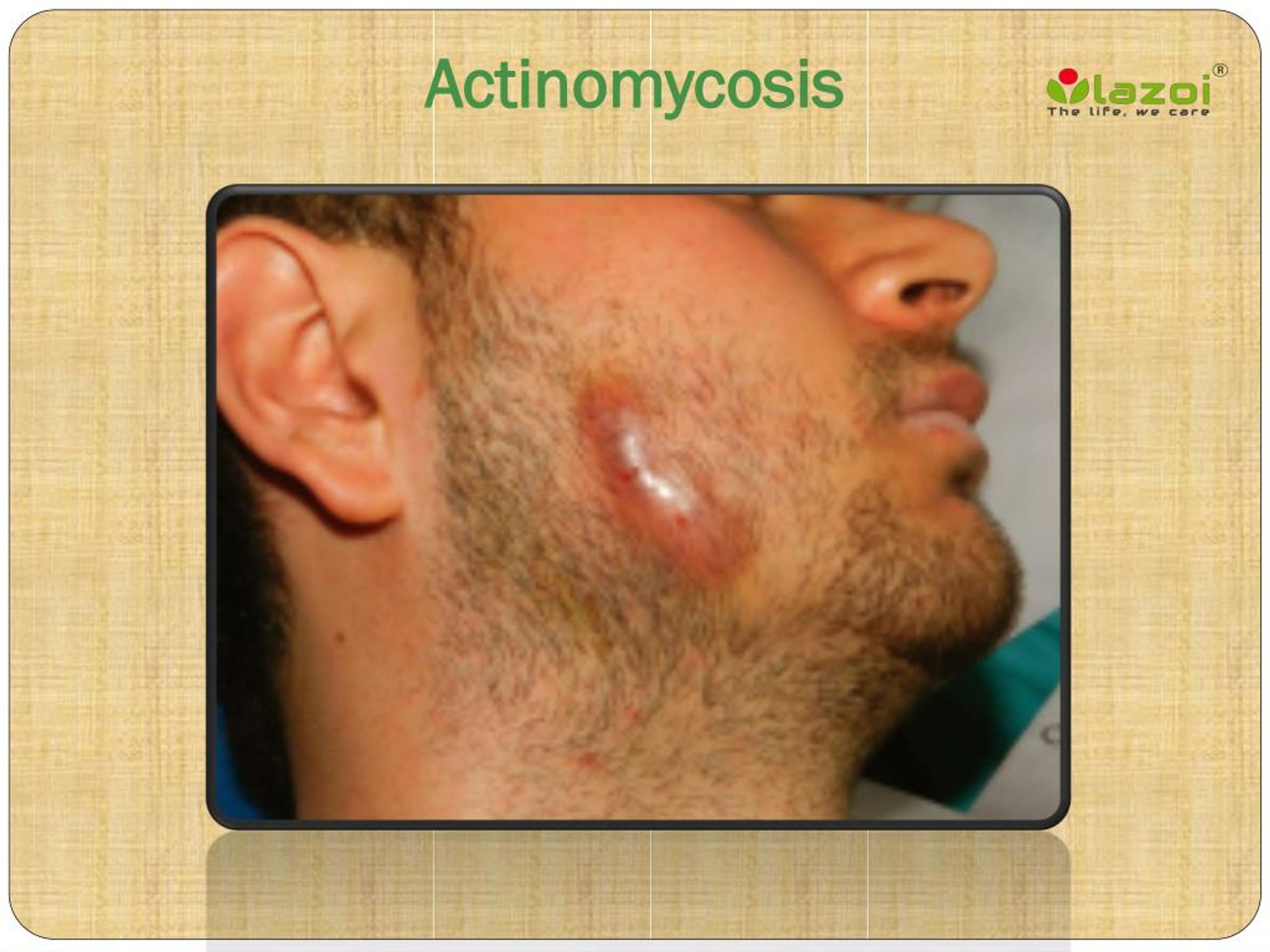
Actinomycosis, a chronic, suppurative and granulomatous disease, is caused by bacteria belonging to the genus Actinomyces. These bacteria are typically found in the nose and throat and often do not cause disease under normal circumstances. However, when they breach the mucosal barriers, such as through surgical procedures, trauma, or poor dental hygiene, they can lead to infection. The disease is characterized by the formation of abscesses, fistulas, and the destruction of tissue. The most common location for actinomycosis is the cervicofacial region (face and neck), followed by the thoracic and abdominal regions. Pelvic actinomycosis, while rarer, can occur, especially in women.
Diagnosing actinomycosis can be complex. Healthcare providers must consider a patient's symptoms, medical history, and perform various tests. A sample of fluid or tissue is often taken to look for the presence of Actinomyces bacteria or the granules they produce. Due to the similarities between actinomycosis and other conditions, such as cancer and anaerobic pulmonary abscesses, doctors may have to perform several tests to confirm the diagnosis.
The management of actinomycosis frequently involves prolonged courses of antibiotics. In more complicated cases, such as those involving infections in critical spaces, massive hemoptysis, or extensive abscesses, surgical intervention may also be necessary. Recovery can be a lengthy process, emphasizing the importance of prompt and accurate diagnosis.
Here's a table summarizing key information about Actinomycosis:
| Aspect | Details |
|---|---|
| Definition | A rare, chronic, suppurative and granulomatous bacterial infection. |
| Causative Agent | Primarily Actinomyces israelii and other Actinomyces species. |
| Typical Locations | Cervicofacial (face and neck), thoracic, abdominal, and pelvic regions. |
| Entry Points | Disruption of mucosal barriers through surgery, trauma, poor dental hygiene, etc. |
| Symptoms | Abscesses, scar tissue, fistulas, chronic inflammation, potentially mimicking cancer or other infections. |
| Diagnosis | Based on symptoms, physical examination, and laboratory identification of Actinomyces in samples of fluid or tissue. |
| Treatment | Prolonged courses of antibiotics; surgical intervention may be necessary in complicated cases. |
| Duration of Symptoms (at diagnosis) | Often approximately 2 months. |
| Key Features | Chronic, localized or hematogenous anaerobic infection; can mimic lung cancer or anaerobic pulmonary abscess. |
| Distinctive Characteristic | Formation of draining sinuses and the presence of "sulfur granules" in pus. |
| Risk Factors | Poor oral hygiene, dental procedures, trauma to mucosal surfaces, IUD use (for pelvic actinomycosis). |
| Complications | Disseminated disease, involvement of critical spaces (e.g., brain abscesses, epidural infections), massive hemoptysis. |
| Prognosis | Generally good with appropriate treatment, but recovery can take time, and complications can arise if diagnosis and treatment are delayed. |
Actinomycosis is often misdiagnosed due to its varied presentation and the similarity of its symptoms to those of other conditions. Thoracic actinomycosis, for instance, is frequently mistaken for lung cancer. This underscores the importance of a thorough diagnostic process, including obtaining samples of sputum, pus, or tissue, to check for specific species of Actinomyces.
The bacterium Actinomyces israelii is exquisitely sensitive to penicillin, which remains a primary treatment option. However, because of the chronic nature of the disease, prolonged antibiotic treatment is usually necessary. The course of treatment can vary, depending on the extent and location of the infection.
In cases of cervicofacial actinomycosis, the infection often presents after oral surgery or due to poor dental hygiene, which allows the bacteria to enter through microfissures. Thoracic and abdominal forms may present differently and can be more difficult to diagnose. Pelvic actinomycosis, while less common, has been observed, and it is particularly relevant to consider its association with certain medical devices like IUDs.
Its also worth noting that marked constitutional symptoms, such as fever, weight loss, and fatigue, may be a later sign, that could indicate a more advanced or disseminated form of the disease. Therefore, early detection, based on careful assessment of clinical symptoms combined with diagnostic laboratory tests, is essential.
The diagnostic process often involves inserting a needle through the skin to obtain a sample from an abscess or infected tissue. The sample is then examined under a microscope by a pathologist to identify the presence of Actinomyces or the characteristic granules. While the disease itself is rare, its potential for serious complications makes it critical to identify it promptly.
Understanding the bacteria's natural habitat and how it interacts with the body is key to understanding actinomycosis. The main niche for Actinomyces is the oral cavity and pharynx. From there, it may spread to different anatomical areas, progressing through tissue planes without respect for anatomical barriers. The presence of abscesses and the formation of fistulous tracts are the hallmarks of the disease. This often leads to confusion with other conditions like cancer, given that its presentation may be similar.
As a result, patients who present with abscesses, scar tissue, or fistulas that suggest actinomycosis are often suspected of having the disease. The diagnostic process is typically initiated when a healthcare provider suspects that the patient's symptoms align with the possibility of an actinomycotic infection. In these situations, the medical staff will carry out specific diagnostic procedures to ascertain whether the condition is present.
The development of actinomycosis is influenced by various factors that allow bacteria to infiltrate body tissues and cause an infection. The bacteria normally reside on the mucosal surfaces of the body. Entry into deeper tissue can occur through surgical procedures, trauma, or conditions that compromise the body's natural defenses.
Although antibiotic treatment is the cornerstone of therapy, the nature of the disease and the possibility of its spread necessitates ongoing monitoring and care. Often, treatment continues for several weeks, or even months, to eradicate the infection completely and prevent recurrence. In some situations, the implementation of antibiotic therapy might need to be coordinated with surgical interventions to improve the outcome. Thus, the management of actinomycosis frequently involves a multi-disciplinary approach.
Therefore, a comprehensive diagnostic and therapeutic approach, taking into consideration the diseases potential to masquerade as other conditions, can significantly improve outcomes.